900 319 0030
enquiry@shankarias.in
What is the issue?
How does the Coronavirus express itself?
What is the RT-PCR method in testing?
What is the principle behind?
How does RT-PCR work in Coronavirus case?
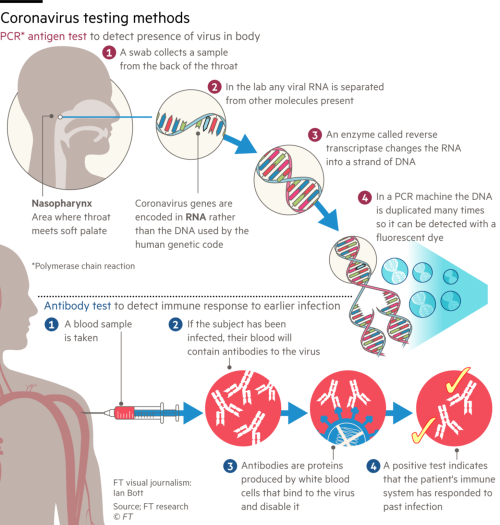
What is the anti-body test?
What are the drawbacks in anti-body test?
Why are both tests relevant now?
Source: The Print, IAEA